Más Información

“Vamos a dar apoyo a los pequeños agricultores por sequía en Sonora”; Claudia Sheinbaum instruye a Berdegué

Derrota de México en disputa por maíz transgénico contra EU; estos son los argumentos de Sheinbaum y AMLO para prohibirlo
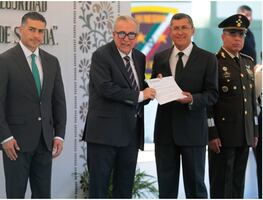
Óscar Rentería Schazarino, ha operado contra CJNG, Viagras y Templarios; es el nuevo secretario de Seguridad en Sinaloa

Claudia Sheinbaum pide respeto para Maru Campos; gobernadora anuncia acuerdo para transporte público

Claudia Sheinbaum anuncia los Centros de Cuidado Infantil en Chihuahua; inaugura hospital en Ciudad Juárez
Every time José Antonio Delgado received a call, he knew he had to get a move on. “We had to go at full speed to reach the area of the country where the outbreak was taking place. Sometimes we went on a Jeep but if we needed to go farther or reach a very remote location, we had to use a chopper,” remembers the doctor while talking about his work in Guinea during the Ebola epidemic which ravaged West Africa between 2013 and 2016.
“I went to Guinea during six weeks with the Spanish mission of the European Center for Disease Prevention and Control (ECDC) but the World Health Organization (WHO) ended up hiring me and I spent one year over there,” says Delgado during an interview with EL UNIVERSAL .
When the epidemic spread across the West Africa, killing 11,000 people, the international community was unable to stop the outbreak given the lack of resources of the continent, both in trained staff and technical resources. Delgado, who was born in Mexico City and studied Medicine at the La Salle University in Mexico, spent three years training in Europe and received his Spanish residence permit in 2008. He was working in a Spanish hospital in Elche, Alicante when he volunteered for the expedition of the ECDC and in may 2015 he traveled to Guinea.
“When I arrived, the outbreak was at its peak. I then began to work for the WHO and developed a decision tree so doctors could discard other diseases when patients arrived with early symptoms of Ebola. There are symptoms, such as high fevers, which can be confused with other diseases such as Malaria, and I developed a method to determine a diagnostic,” explains Delgado.
The doctor lived in the Forecariah region of Guinea. From there, he coordinated 40 epidemiologists and moved constantly whenever new outbreaks were registered. Once the epidemic was controlled, he focused his efforts on border control so the sick couldn't cross unchecked between Guinea and Sierra Leone .
The workload, fear of contagion, and political instability of Guinea have led Delgado to call the year he spent in the country as “very stressful” but remembers it as one of his greatest and most vital professional experiences, as he contributed to controlling one of the worst epidemics in recent times.
“Studying Medicine in helped me, as well as the experience I got from my social service during the internship,” explains the doctor from his new position at the Epidemiology Unit in the Conselleria de Sanitat Valenciana.
One of the most complicated aspects of his mission was developing a relationship with the local population. “Villagers were nervous and very afraid. The virus was lethal and many had lost their relatives and felt intimidated by foreigners,” he recounts.
Whenever there was a new outbreak, foreign health officials quarantined the population. “For a society highly dependant on family ties, it was very hard for them to see one of their family members being taken away, sometimes never to return,” he says, telling us how the cultural difference made the epidemic harder to control. “When someone dies, they have the custom of washing the body and celebrating a massive funeral. This was a medical disaster because the viral load at the time of death is at its maximum, so the disease spreads quickly. That is why we had to intervene. We couldn't allow people touching the bodies and we made sure they were all buried,” describes Delgado.
In January 2016 the end of the epidemic was finally declared and on April 30 Delgado returned with most of the international aid. Only a few remained to take care of the aftermath of the plague and help treat – mostly – depression and stigmas on survivors.
“We did good work over there and this allowed African protocols and services to improve yet this isn't a long-term work. People are still vulnerable and they could suffer the effects of a new epidemic,” he adds.
A year and a half after his return to Spain , and after recovering from such a grueling experience, Delgado claims he would like to return to Africa. “It's a door which always remains open. I'm in the database of the WHO and they can always call me. It's a very attractive experience, although it is true that having a job [in Spain] makes it complicated,” he adds.
am





